The Ultimate Osteoporosis Course for Health Practitioners & Passionate Laypeope
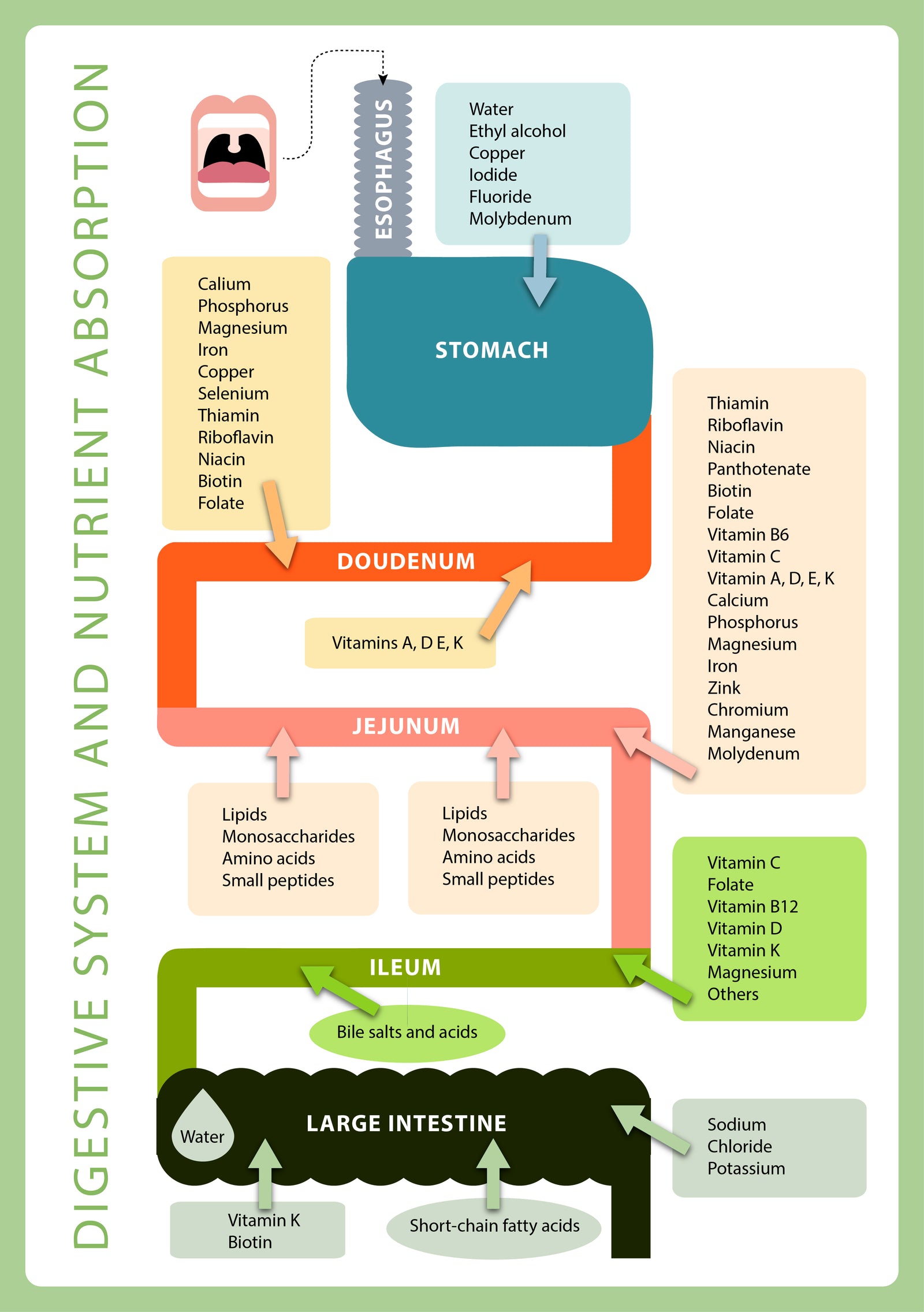
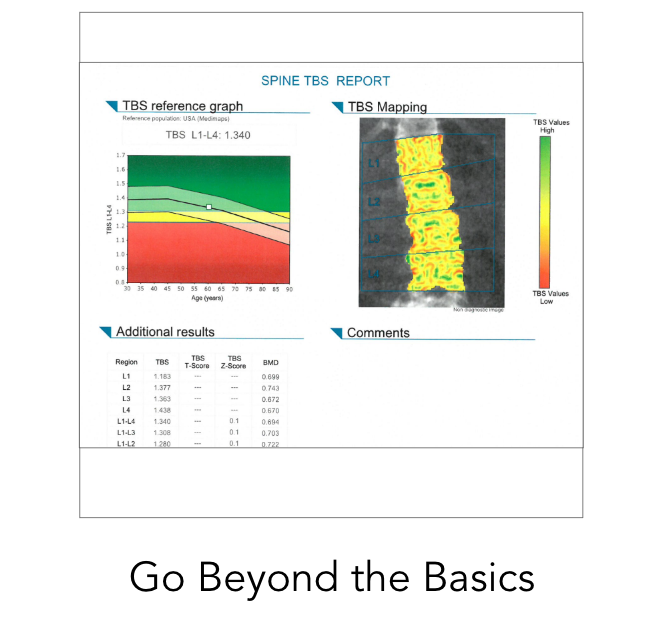
It's finally here! In my 20 hour comprehensive Ultimate Osteoporosis Course you'll understand how bone density scans, labs, and gut health work together to impact bones and osteoporosis. We work with actual case studies to customize prevention plans, learn how interpret DXA's and labs, and diagnose with confidence. We’ll go deep and wide and tackle all things bone health—for you and everyone you care about. Join us if you are ready to take your learning to the next level. Click Here To Learn More
The Osteoporosis Fundamentals Bundle consists of our three favorite classes on the most-asked questions: Can I treat my osteoporosis naturally? Do I need medication? What medications are there?
This package is perfect for people looking for clarified, well-researched information on this complex condition and treatment options.
Limited time offer at $35.00!
“Balanced and fair in her approach to treatment, Dr. Simpson discusses dietary changes, exercise options, supplements, and medication. Along the way she has made the complex topic of bone metabolism approachable and relevant. An important read for providers and patients alike, or as she says, ‘anyone with a skeleton.’”
— Robert Purchase, MD Orthopedic Surgeon
Exclusive Master Class: Dr. Lani and Specialists on the latest in bone health
In my weekly master class, you'll gain knowledge of the key areas that help you improve your overall bone health! Members have the opportunity to receive personalized insights from me and my featured experts.
Learn More

Featured In